Yet most of us, particularly the elderly, are unaware of the malnutrition risk
- Malnutrition costs the health and social care service an estimated £23.5 billion each year[1]
- Half of us cannot identify symptoms and a third aren’t confident seeking help
- Over 65s at risk, with many reporting worsening health and diets, but 9 in 10 unconcerned about developing malnutrition
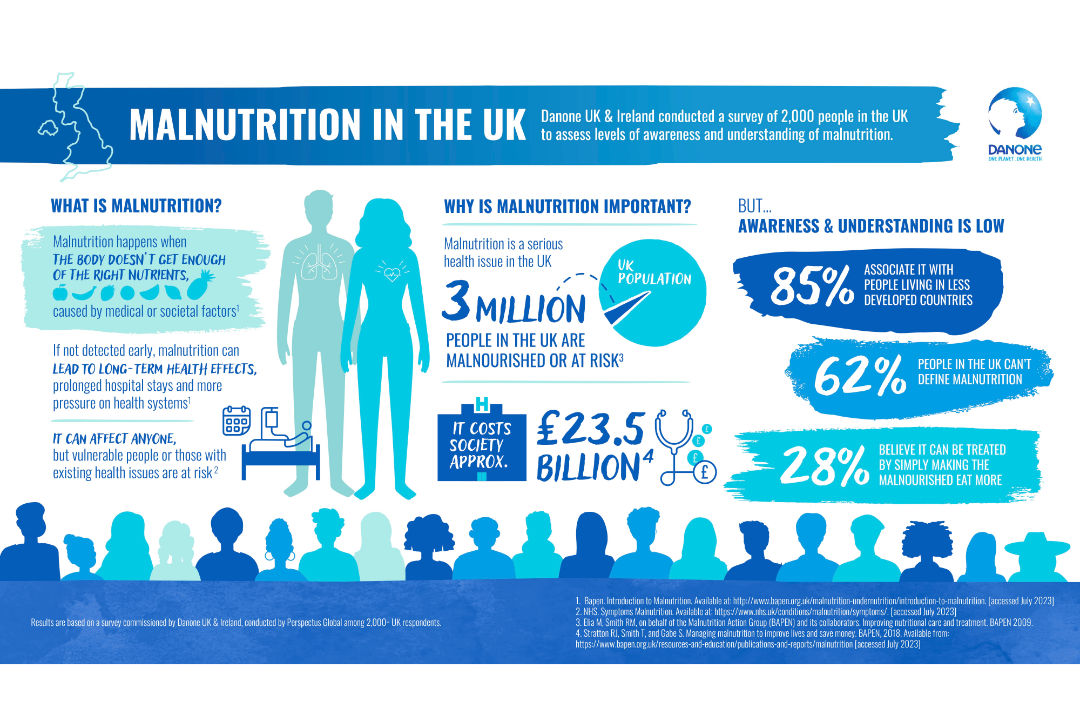
Despite 85% of people thinking malnutrition only occurs in less developed countries, it is one of the UK’s biggest blights. A staggering 3 million people are malnourished or at risk,[1] costing society an estimated £23.5 billion every year,1 while adding to existing strains and creating a huge burden for the health system. New research published today from Danone UK & Ireland reveals half of the public cannot spot symptoms, a third don’t know where to seek help, and older people show little concern despite being at higher risk. If left unchecked, malnutrition risks becoming a ticking timebomb for the health of the nation.
The research found malnutrition is heavily misunderstood by the public, with more than three-fifths (62%) not able to define it. Malnutrition is when the body doesn’t get enough of the right nutrients, in the right amounts. Often this can be down to existing diseases or illnesses. While disease is a key driver, social and economic factors can also contribute to the risk of developing malnutrition, particularly if a person is not able to access or incorporate foods that provide necessary nutrients in their diet. [2]
If not identified early, malnutrition can lead to disease complications, prolonged hospital stays and can have long-term health effects,3 yet a third of respondents (31%) are not confident knowing how to get support for a loved one who may be malnourished. A third (28%) also thought that simply making the malnourished eat more is a quick fix, when in practice, treatment is more complex and resource intensive for the health system.
More than half of the public (54%) incorrectly thought fainting and seizures were key indicators of someone suffering from malnutrition, while two-fifths (40%) thought abdominal cramps were, and a third (34%) incorrectly believed jaundice was a sign. In reality, key symptoms can include unintentional weight loss, loose fitting clothing or feeling weak.[3]
Older people are particularly vulnerable with over a million over-65s estimated to be malnourished.[4] However with screening for malnutrition low across the UK, figures could be even higher. Up to one in three over-65s admitted to hospital for other conditions are at risk of malnourishment[5]. Alarmingly, the research shows that the vast majority (92%) of over 65s say they do not worry about becoming malnourished.
Worryingly, the research found that 66 is the age when older people are more likely to lose interest in eating healthy, nutritious meals, while half (50%) of over 65s admit they do not eat as much fresh fruit and vegetables. In fact, more than one in 10 (14%) say their diet has become less healthy than it was last year. Over a quarter (28%) of over-65s report this change in diet has left them more vulnerable to illness, creating or exacerbating existing health problems.
The study also found that a fifth (17%) of over 65s are skipping at least one meal a day, while a further 23 percent forgo meals once a week. This was attributed to older people saying they rarely feel hungry or have lost their appetite (31%). Changes in appetite can occur in older age for various reasons[6] but can also be a symptom of malnutrition.4
A fifth (19%) said they were trying to save money with 14 percent saying food is expensive. This finding is concerning when considering that people with long-term illnesses are more likely to be financially worse off already[7] and people with existing health conditions are already susceptible to the risk of malnutrition.
Commenting on the research, GP and TV medic Dr Amir Khan said “The research from Danone UK & Ireland shows a worrying lack of awareness about the hidden and serious problem of malnutrition, which continues to grow and puts a significant strain on the NHS. It’s not an easy condition to spot, but early detection is key and will reduce the chances of further deterioration and hospital admission. So, if you have a loved one you’re concerned about who may be growing more frail, or has had a dramatic change in eating habits or difficulty swallowing, then make sure you speak to a health professional or carer, particularly if they have a pre-existing condition.”
Danone UK & Ireland is highlighting the need for screenings and management to be available for those who may be at risk of being malnourished.
As a nurse for Nutricia, Danone’s medical nutrition arm, for over eight years, Ann Fazackerley, Clinical Practice Manager at Danone UK & Ireland has directly supported patients who are malnourished. Speaking on the scale of the issue she commented: “I’m passionate that there needs to be more understanding about the causes, detection and prevention of malnutrition, which affects people of all ages. More needs to be done to find effective solutions that properly address the malnutrition crisis in the UK, including standardised screening across healthcare settings. If we were able to tackle malnutrition at an earlier stage this would reduce the burden on the patient and the health system.”
Lesley Carter, Programme lead of the Malnutrition Taskforce and Head of Professionals and Practice, Health Influencing at Age UK added: “While there’s been progress in tackling preventable malnutrition, a lot more needs to be done. It is essential to get to grips with the symptoms early and have a better awareness of unplanned weight loss, whether it is brought on due to an existing illness or as a result of social issues. Malnutrition is dangerous for older people, particularly those living in the community who may also have underlying long-term conditions and other health needs. It’s very important that we all know how to recognise the signs of malnutrition and know what to do to prevent it and how to treat it. Having conversations with older people to learn about their challenges to access, prepare and eat food will do so much to prevent malnutrition in the community and unplanned hospital admissions.”
References
[1] Stratton RJ, Smith T, and Gabe S. Managing malnutrition to improve lives and save money. BAPEN, 2018. Available from: https://www.bapen.org.uk/resources-and-education/publications-and-reports/malnutrition [accessed July 2023]
[2] Elia M, Smith RM, on behalf of the Malnutrition Action Group (BAPEN) and its collaborators. Improving nutritional care and treatment. BAPEN 2009.
[3] Bapen. Introduction to Malnutrition. Available at: http://www.bapen.org.uk/malnutrition-undernutrition/introduction-to-malnutrition. [accessed July 2023]
[4] NHS. Symptoms Malnutrition. Available at: https://www.nhs.uk/conditions/malnutrition/symptoms/. [accessed July 2023]
[5] Malnutrition Task Force. State of the Nation. Available at: https://www.malnutritiontaskforce.org.uk/sites/default/files/2021-10/State%20of%20the%20Nation%202020%20F%20revise.pdf. [accessed July 2023]
[6] Malnutrition in England Factsheet. Available at: https://www.malnutritiontaskforce.org.uk/malnutrition-england-factsheet. [accessed July 2023]
[7] Malnutrition Task Force. Eating Well in Later Life. Available at: https://www.malnutritiontaskforce.org.uk/sites/default/files/2019-10/LR%208202%20Age%20UK%20Malnutrition%20TF%20-%20Eating%20well%20in%20later%20life%20booklet%20A5.pdf. [accessed July 2023]
[8] The Health Foundation. Living in poverty was bad for your health long before COVID-19. 25 July 2020. Available at: https://www.health.org.uk/publications/long-reads/living-in-poverty-was-bad-for-your-health-long-before-COVID-19. [accessed July 2023]
Notes to editors:
The survey was conducted by Perspectus Global among 2,000+ UK respondents.
